#Marr: Is the coronavirus under control?
— BBC Politics (@BBCPolitics) December 20, 2020
Health Secretary Matt Hancock: "No. It’s not. The new variant is out of control"https://t.co/gxUy3acCro pic.twitter.com/IWYQ2fKVOW
The opinions expressed on this website are that of my own and do not reflect that of any employer or commercial organization.
Translate
Sunday, December 20, 2020
New Variant COVID 19
Sunday, December 13, 2020
Stop Surface Cleaning
Now in print. Highly recommend this perspective from 3 leading experts
— Eric Topol (@EricTopol) December 13, 2020
"Shared air is the problem, not shared surfaces"
"No data studies we are aware of have cultured the virus from surfaces" pic.twitter.com/GkBk7F68vf
Friday, December 11, 2020
Myocardial Biomarkers and COVID-19
Respiratory infections are a known risk factor for myocardial infarction (MI), and a self-controlled case series study by Kwong and colleagues sought to quantify this risk. Researchers used a public insurance database in Canada to assess their study question, and their results were published in the January 25, 2018 issue of the New England Journal of Medicine.
There were 364 cases of acute myocardial infarction (AMI) in the one year before and after a positive test for influenza. Rates of AMI during the risk interval 7 days after respiratory specimen collection and the nearly 2-year control interval were 20 and 3.3 admissions/wk, respectively. This resulted in an incident ratio for MI in comparing the two periods of 6.05 (95% CI: 3.86, 9.5). The risk for MI did not increase significantly past 7 days after viral testing.
Influenza A and B were associated with the highest risks for AMI, with rates 5- to 10-fold higher in the risk interval; however, infection with respiratory syncytial virus and any other virus were still associated with a higher risk for MI compared with the control period.
Coronavirus disease 2019 (COVID-19) has also been associated with myocardial damage and thrombosis. The current study quantified incident myocardial damage associated with COVID-19 and how such damage may affect patient survival.
Summary:
- A previous study by Kwong and colleagues found that rates of AMI were substantially higher in the 7 days after a respiratory viral infection. Although infection with influenza was associated with the strongest increase in the risk for MI, infection with any respiratory virus was associated with a higher risk for MI as well.
- The current study by Giustino and colleagues demonstrated that 62.6% of patients admitted for severe COVID-19 had elevated serum troponin levels, and most patients with myocardial injury had abnormal findings on TTE. The combination of myocardial injury and abnormal TTE was associated with a higher risk for in-hospital mortality.
- The healthcare team should remain aware of the risk for cardiac involvement among patients with severe COVID-19 and the combination of abnormal troponin levels and TTE findings suggest a worse prognosis.
Tuesday, December 8, 2020
Beyond the Basics of Cardiac Amyloidosis: Pearls and Pitfalls of Imaging and Diagnosis
This a great lecture , with Dr. Rodney Falk who dedicated his entire career on the research of amyloidosis- realize that you probably miss AL , but especially ATTRwt amyloid very frequently in the ICU- this is NOT a rare disease anymore ( see earlier postings ). It is also the diagnosis mostly frequently missed by Cardiologists ( discusssed in the lecture ) .
Monday, December 7, 2020
An Approach to Mechanical Heart Lung Interaction
Heart Lung Interactions in CCM (link to website heart-lung.org )
Jon-Emile S. Kenny M.D, M.Sc
Chief Medical Officer of Flosonics Medical in Toronto, Canada.

Tuesday, November 24, 2020
Advanced Management of Intremediate -and High -Risk Pulmonary Embolism
Advanced Management of Intermediate- and High-Risk Pulmonary Embolism JACC Focus Seminar https://t.co/dFCEmslvy7
— Guy De Gent (@gdegent) November 24, 2020
You will find a link to Papers,where I store my complete files and articles , https://app.readcube.com/
Friday, November 13, 2020
Atrial fibrillation and COVID-19
Tuesday, October 27, 2020
Overtreatment in Medicine
Wednesday, September 9, 2020
Tuesday, September 8, 2020
RIP-Laika
Although this really doesn't belong as an entry in my blog, in a way it does as Laika and other animals contributed to exploring and recognizing our space in the cosmos . It also refers to the title of the blog.
from WIRED :
Space Dogs uses archival footage to tell the story of the clever, docile, and doomed Moscow street dog Laika, the first mammal to go into orbit—and the first mammal to die there. In 1957, the Soviet Union sent Laika to space in the satellite Sputnik 2. Despite initial assurances to the public that the pup would come back unharmed, she was always intended as a sacrifice to scientific progress, as there was no way to return her to Earth at the time. For years, the party line from officials was that Laika had been humanely euthanized before the satellite reentered the atmosphere. In reality, she lasted less than a day before heat and stress killed her, turning the object of cosmic progress into her small coffin. The film doesn’t have footage of Laika suffering in space (thank God) but it does have plenty of clips of scientists putting Laika and a few other research dogs through a barrage of exercises—they spin in a centrifuge, dazed—and subjecting them to invasive, gruesome surgeries in order to rig them up with the necessary sensors to see how long they’d last alone above the planet’s atmosphere.
It is not a pleasant viewing experience. In fact, if I had to imagine the film I would least like to be forced to watch, Clockwork Orange-style, with my eyes pried open, it might be this one. It is a stylish and honest film—a rare combination!—but also merciless
Space Dogs from Icarus Films on Vimeo.
The ACTS Randomized Clinical Trial
Now we got three decently-sized randomized controlled trials, all in agreement: vitamin C does not reverse organ failure in sepsis," commented critical care physician Robert Dickson, MD, of the University of Michigan School of Medicine in Ann Arbor.
The VITAMINS trial showed no advantage in recovery from septic shock and numerically higher mortality with a vitamin C-hydrocortisone-thiamine combination. The CITRIS-ALI trial showed no impact on SOFA scores from high-dose IV vitamin C.
"If the signal of benefit for vitamin C was anywhere near as strong as was initially suggested, it shouldn't be this hard to detect it in clinical trials," Dickson added.
The researchers noted that vitamin C has also been proposed for treating respiratory failure from COVID-19, as was seen in a recent case report.
However, Dickson said, "the data supporting use of vitamin C in sepsis were already weak. The data supporting its use in COVID-19 are non-existent."
Any excuses Paul Marick after belittling the primary investigator of the Vitamins Trial?
Ref: Kamagurka
Friday, July 3, 2020
Cytokine Storm Nothing but a Tempest in Teapot?
Severe COVID-19 is associated with deep and sustained multifaceted cellular immunosuppression https://t.co/CpbQRnVFAI
— Guy De Gent (@gdegent) July 4, 2020
9/5/2020. Here is more data from theUniversiteit van Nijmegen in Holland that cytokine storm probably is not part of SARSCov2 infection, as already written earlier in this post, I can't recall ever seen one clinically. As a matter a fact we maybe doing the complete wrong intervention by suppressing the immune system .Tociluzimab is even given from day one by some institutions with Remdesivir, biologically that makes no sense.
Their Conclusion :
"In this study, critically ill patients with COVID-19 with ARDS had circulating cytokine levels that were lower compared with patients with bacterial sepsis and similar to other critically ill patients. These findings are in line with lower leukocyte counts observed in patients with COVID-19, and are possibly due to lower overall disease severity, despite the presence of severe pulmonary injury. The findings of this preliminary analysis suggest COVID-19 may not be characterized by cytokine storm. Whether anticytokine therapies will benefit patientswith COVID-19 remains to be determined."
Thursday, July 2, 2020
Covid-19 deadlier than acute myocardial infarction
This figure (via @ScottGottliebMD) receiving a lot of attention— Ashish K. Jha (@ashishkjha) June 28, 2020
And folks rightly point out mortality rates lower for young than for elderly
But thats true for every disease
So as point of reference:
How do these rates compare to mortality for folks with heart attack?
Thread pic.twitter.com/Vw1mtCcXCE
Tuesday, June 30, 2020
Saturday, June 27, 2020
Anticoagulation Management COVID-19
Link to SCCM article on coagulopathy in COVID -19
Thromboelastographic Results and Hypercoagulability Syndrome in Patients With Coronavirus Disease 2019 Who Are Critically Ill
• All patients with COVID-19 should undergo coagulation studies at admission, in particular:
D-dimer, prothrombin time, and platelet count.
• Because of the possibility of patients to develop coagulopathy later in their hospital course,
routine serial measurements of coagulation studies should be undertaken in all COVID-19
patients. The ideal interval has not yet been defined .
• All patients with COVID-19 should be placed on prophylactic doses of anticoagulation,
preferably with LMWH, unless there is a contraindication, such as acute kidney injury (AKI),
wherein unfractionated heparin is preferred.
• Therapeutic anticoagulation should be strongly considered in patients at high-risk for
coagulopathy (including CRRT and ECMO), demonstrating signs of microthrombi-induced
organ dysfunction, or with documented or strongly suspected macro-thromboembolism.
Determination of high-risk patients by laboratory measures of coagulopathy may include:
platelet count, prothrombin time, fibrinogen, fibrinogen-degradation products, D-dimer,
and TEG. Of note, some centers are therapeutically anticoagulating all patients on
admission when no absolute contraindications exist.
• Given the significant rate of AKI seen in COVID, intravenous contrast for imaging should be
used with caution. Duplex ultrasonography, echocardiography, and clinical suspicion can
play an increased role in these cases.
• Some early reports support extended-infusion tPA as a potential approach to refractory
cases
• Aspirin should be considered in cases with elevated troponin and cardiac dysfunction,
particularly with elevated maximal amplitude on TEG.
Conclusions Lancet study on TEG:
COVID-19 patients in the intensive care unit (ICU) demonstrated venous thromboembolism (VTE) in 27%, and arterial thrombosis in 3.7%.
Investigators observed the TEG parameter for lysis at 30 minutes (LY30) was statistically significantly linked to VTE, with an AUROC of 0.742 (P = .021). The TEG α-angle and D-dimer were significantly associated with new onset need for dialysis (0.771 [P = .035] and 0.779 [P = .005], respectively).
"As a rapid test to demonstrate complete fibinolysis shutdown, an LY30 of 0% in conjunction with D-dimer levers of 2600ng/ml may serve as a sensitive marker for the patients most at risk for VTE and other thrombotic complications," Wright and colleagues concluded.
• Because of the possibility of patients to develop coagulopathy later in their hospital course, routine serial measurements of coagulation studies should be undertaken in all COVID-19 patients. The ideal interval has not yet been defined .
• All patients with COVID-19 should be placed on prophylactic doses of anticoagulation, preferably with LMWH, unless there is a contraindication, such as acute kidney injury (AKI), wherein unfractionated heparin is preferred.
• Therapeutic anticoagulation should be strongly considered in patients at high-risk for coagulopathy (including CRRT and ECMO), demonstrating signs of microthrombi-induced organ dysfunction, or with documented or strongly suspected macro-thromboembolism. Determination of high-risk patients by laboratory measures of coagulopathy may include: platelet count, prothrombin time, fibrinogen, fibrinogen-degradation products, D-dimer, and TEG. Of note, some centers are therapeutically anticoagulating all patients on admission when no absolute contraindications exist.
• Given the significant rate of AKI seen in COVID, intravenous contrast for imaging should be used with caution. Duplex ultrasonography, echocardiography, and clinical suspicion can play an increased role in these cases.
• Some early reports support extended-infusion tPA as a potential approach to refractory cases
• Aspirin should be considered in cases with elevated troponin and cardiac dysfunction, particularly with elevated maximal amplitude on TEG.
Conclusions Lancet study on TEG:
COVID-19 patients in the intensive care unit (ICU) demonstrated venous thromboembolism (VTE) in 27%, and arterial thrombosis in 3.7%.
Investigators observed the TEG parameter for lysis at 30 minutes (LY30) was statistically significantly linked to VTE, with an AUROC of 0.742 (P = .021). The TEG α-angle and D-dimer were significantly associated with new onset need for dialysis (0.771 [P = .035] and 0.779 [P = .005], respectively).
"As a rapid test to demonstrate complete fibinolysis shutdown, an LY30 of 0% in conjunction with D-dimer levers of 2600ng/ml may serve as a sensitive marker for the patients most at risk for VTE and other thrombotic complications," Wright and colleagues concluded.
Saturday, May 9, 2020
Money Isn't Everything
How were Kerala, India and Vietnam so successful vs #COVID19?— Eric Topol (@EricTopol) May 8, 2020
“Countries that took early, aggressive action, using proven methods, have severely limited the virus. ..if you reduce fast enough, you never reach the point of exponential growth.” @toddmpollack https://t.co/5oWeISdNu7 pic.twitter.com/VJ19ZAkbtA
Thursday, April 2, 2020
Friday, March 13, 2020
Severe SARS CoV-2 diagnosis, CT Chest Findings and Management Strategies for the Intensivist
Above are data from Wuhan.
additional CT resources from Belgium and Wuhan
Sunday, March 8, 2020
Thursday, February 27, 2020
The Effect of Xenobiotics on the EKG
Wednesday, February 12, 2020
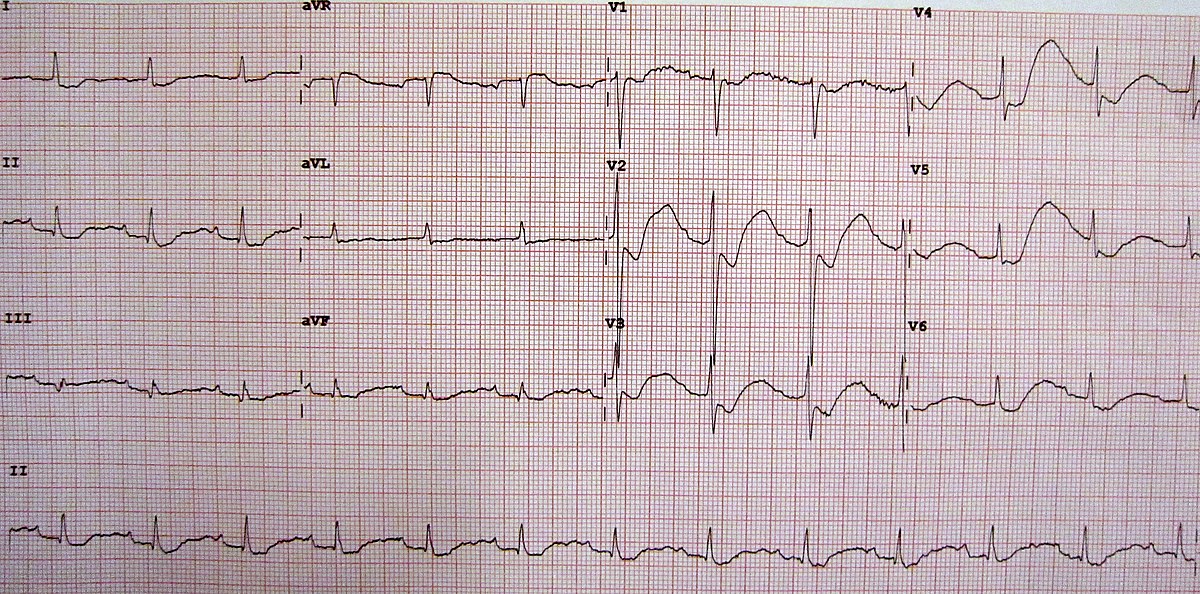
ST-Elevation on the ECG in a 36 year old man (Presented at ESC Congress 2019)
Tuesday, January 28, 2020
How to calculate actual risk of Torsades des Pointes with QT prolongation
- FACT: Computer generated QT/QTc calculations are unreliable and should not be used.
- Measure QT manually( yes use calipers!)

- There is no common agreement which QT value to use, I prefer to use the longest QT, but other advocate average of all leads( time consuming and QT cannot be measures usually in all leads), or use lead II ( QT can be measures) as this is lined up with mean QRS vector.
- Calculate QTc according to Fredericia or Hodges formula ( Bazzett's formula over corrects QTC at higher heart rates often present in critically ill patients).
- Example
- For the above example the measured QT in leads I, II aVF, V2, V4, V6 are 320, 340, 320, 300, 340 and 320 respectively. This gives a median QT of 320ms. Note the computer generated QT is longer at 360ms, correcting with Bazett’s formula to 485 – which would be considered prolonged. However plotting this on the nomogram shows a level which is well below the risk line. Bazett’s QTc over corrects in tachycardia and under corrects for slow heart rates and should not used in toxicology patients to determine overall risk of TdP.
- The QT nomogram has a sensitivity of 97% and specificity of 99% for predicting TdP following toxicological ingestions and has been found to be more accurate in predicting TdP than using Bazett’s QTc of 440ms or 500ms.
Sunday, January 19, 2020
VITAMINS Trial: Vitamin C and Thiamine for Sepsis and Septic Shock
I probably should not make the same mistake as Paul Marik , taking a fanatical view. Usuallly the end result does not turn out in your favor . After reading the paper quickly, there are many problems not in the least the timing of the intervention.
On the other hand, I cannot disagree with his Lacto- Bolus reflex comment and his statement that 30 ml /kg of fluid is a hoax in sepsis .....he actually published this .
Conclusion in my view is there is no conclusion "yet" . I would like to hear other comments. I posted the video of the Vitamins Trial on the blog. Even if your not interested in this trial , with Paul Marik there it is quite entertaining.
Saturday, January 18, 2020
Familial Atrial Fibrillation
Family history: Father had atrial fibrillation when he was 21.
Vital signs blood pressure 117/72 heart rate 62 respirations 20 temperature 98 on room air
Notable labs White count 10.8, hemoglobin 17.2, platelet count 244, d-dimer less than 0.19 mg/L, potassium 3.4, total protein 8.7, TSH 2.55 drug screen negative hepatitis C antibody negative, troponin less than 0.017
Patient likely has familial atrial fibrillation:
This is an autosomal dominant disorder .The first single gene found to be associated with familial atrial fibrillation was KCNQ1, which provides instructions for making a channel that is embedded in the outermembrane of cardiac muscle cells.
How would you treat such a young patient ?
Get stat echocardiogram to rule out structural heart disease, obstructive coronary artery disease would be extremely unlikely, check TSH and if patient he has no structural heart disease would give 300 mg of flecainide PO x1, type Ic antiarrhythmic on Cardizem, after correction of all electrolytes and likely patient will cardiovert back to normal sinus rhythm as new onset.
Would watch patient for 4 hours for pro-arrhythmias. Patient can then be discharged same day and given instructions on how to use pill in the pocket approach [i.e take 300 mg of by mouth flecainide ×1 or 600 mg propafenone, but the latter has also beta blockade effect, while on either a beta-blocker or calcium channel blocker]. I would not put the chronically on an antiarrhythmic drug, especially note amiodarone, but continue Cardizem after his converted.
Never give a type Ic antiarrhythmic without use of either calcium channel blocker or beta-blocker prior to given flecainide or propafenone. This can lead to one-to-one conduction and ventricular rate of 300 bpm and cardiac arrest secondary to V. fib
Beta-blockers are usually not well tolerated in young men This approach would also avoid any need for anticoagulation at any point. It is a real case with the patient came in on Saturday morning, but then approach was chosen to keep him until Monday morning for possible electrical cardioversion if he did not spontaneously convert with Cardizem IV/by mouth beta-blocker . The downside of this approach is that the patient is for at least 2 days in the hospital if not 3.
If an episode happens again he will have to come back to the emergency room, while with the above approach he can treat himself.
Obtain a single lead tracing at the time of atrial fibrillation and another one after he has converted and forward tracings to his physician. If he does not convert then he can go to the emergency room.
Therefore I always recommend for the patient to obtain an AliveCor monitor so he can tell when is in atrial fibrillation and can forward this in a HIPAA compliant way to his cardiologist.
There is no reason reason to follow this with an apple watch and more expensive devices.
Presenting this case not so much from the perspective of familial atrial fibrillation, although this is also an interesting observation. In this vignette , like to point out why we have such an expensive health care system. I am not sure how a case like this would be handled in Europe now, but doubt the patient would have to stay overnight. Now you are talking about 2-3 days in the hospital, possible electrical cardioversion and no future on hand treatment for the patient if this should recur in a couple of weeks requiring trip back to the ER.
Monday, January 13, 2020
Risk Stratification of Arrhythmia in DCM
Some commercial kits now have testing for 176 genetic markers.
Worth a watch !
Causes of Hyponatremia: Does This Patient Have Pseudo-Hyponatremia ?
Anion gap = 14, glucose = 247 mg percent, sodium = 109 mEq per liter, potassium is 4 mEq per liter bicarbonate = 16 mg/L, chloride 100 mg/L, BUN is = 7 mg percent, creatinine < 0.4 mg percent
Total protein 5.7 g percent, albumin 4.3 g percent
Total cholesterol = 994 mg percent, HDL = 21 mg percent, LDL less than 3 mg percent, triglycerides 7889 mg percent
2.Are all follow-up sodium levels subjective pseudohyponatremia and values dependent on ongoing insulin therapy?
The answer : 1.NO and 2.NO
The differential diagnosis for pseudohyponatremia includes hyperglycemia with elevated glucose levels typically greater than 400 mg percent, hyperlipidemia and or hypertriglyceridemia and hyper proteinemia seen in multiple myeloma.
There have been many reports in the past of pseudohyponatremia with hypertriglyceridemia and or hyperlipidemia. So why in this example does the patient does not have pseudohyponatremia.It is critical to understand how electrolyte levels are measured in the current laboratory setting and how handling of a lipemic specimen is handled differently currently then has been in the past.
The two different technologies used for the measurement of electrolytes are named in various ways in the literature; however, the most frequently used names are direct ISE and indirect ISE. ISE means ion-selective electrodes.
Indirect ISE:
- Measures on a total plasma sample (or serum) that has been diluted with a large volume of diluent.
- Requires that the plasma and erythrocytes are separated by centrifugation.
- Due to the dilution, this method measures the mean concentration in plasma, i.e. the weighted average between the concentration in the electrolyte-containing water part and in the electrolyte-free protein/lipid part. The concentration is calculated by multiplying the result with the dilution factor.
- The results are comparable to flame photometry.
- This technology is typically used in the large so-called chemistry analyzers in the centralized laboratory.
- The reported result depends of the content of solids in the sample.
Direct ISE:
Measures on a non-diluted whole-blood or plasma sample. However, the actual measurement is performed on the plasma water.
- When whole blood is used, it does not involve any sample preparation.
- Direct ISE actually measures the electrolyte activity in the plasma water (mmol/kg H2O) rather than "concentration in the plasma (mmol/L)". The electrochemical activity of the ions in the water is converted to the readout concentration by a fixed (ion-specific) multiplier. This is only accurate for a given ionic strength, usually chosen to equal 160 mmol/L for plasma.
- The use of this fixed factor ensures that direct ISE reflects the actual, clinically relevant activity, irrespective of the level of proteins and/or lipids. This is not changed by the fact that the result traditionally is termed "concentration".
- This conversion is based on recommendations from the IFCC Expert Panel on pH and Blood Gases and is made in order to avoid the confusion of having two types of electrolytes results.
- This technology is typically used in blood gas analyzers and POC electrolyte analyzers, and these may be placed both in the laboratory and in a point-of-care environment.
- The reported result is independent of the content of solids in the sample.
In conclusion, the results from the two different types of analyzer are brought to correlate for samples with a normal content of proteins and lipids. This, of course, requires that all preanalytical and analytical variations are eliminated.
SAMPLES WITH AN ABNORMAL PROTEIN/LIPID CONTENT
The variation of the content of proteins and lipids from the normal situation will cause an error on the reported electrolyte results from the indirect ISE.
In the literature, it is reported that the error is less than 5 % when triglyceride concentration is less than 2500 mg/dL (recommended level is 35-160 mg/dL). The impact of errors on the measurement of electrolytes applies to all electrolytes; however, it is most pronounced on sodium.
Examples of errors on sodium from the literature: An error of 17 mmol/L is reported with an increased protein content, and an error of 26 mmol/L due to increased lipid content.
When the solid content deviates from the normal, it is typically increased, and the typical types of error are then:
Electrolyte concentration is reported as normal or low when it is actually dangerously high, or
Electrolyte concentration is reported as too low when it is actually normal.
The latter phenomenon is also called pseudohyponatremia where sodium is concerned.
Increased content of protein and lipids is the case for a long list of common medical conditions such as diabetes, liver and kidney syndromes, alcoholism, etc. Due to its magnitude is may lead the physicians to life-threatening erroneous conclusions and should therefore be taken into consideration when evaluating electrolyte results reported from the indirect ISE technology.
Based on the above explanation the patient should have pseudohyponatremia from hyperlipidemia, however, this is not how present day lipemic specimen's are handled. After centrifugation of whole blood, the lipid layer is actually dissolved and solids in the sample do not influence result anymore. The samples are pre-treated with LipoClear. Electrolytes are measured in the clear specimen. See Image below

Therefore,only significant hyperglycemia and hyperproteinemia are more likely then triglycerides to cause pseudohyponatremia. This patient did not have hyperglycemia nor hyperproteinemia. As triglyceride levels fall with insulin therapy, the reported sodium levels will not alter. If they do then the specimen was not handled properly with LipoClear.Ultracentrifugation is the other method if LipoClear is not available to measure electolytes without inference from the lipids .
Featured Post
Fourth Universal Definition of Myocardial Infarction
The following are key points to remember from this Expert Consensus Document on the Fourth Universal Definition of Myocardial Infarction (M...
-
I will write more about this in the next blog, but the concept of driving pressure ( Pdr = Vt/Crs- Vt; tidal volume, Crs; compliance respir...
-
CV Medications in Pregnancy Table for Quick Review, I posted this article earlier in the year but not the Central Illustration Cardiova...
-
Explaining shock index (SI) Shock index (SI) is the ratio of heart rate (HR) to systolic blood pressure (SBP), expressed in beats per minut...